What We Are Seeing
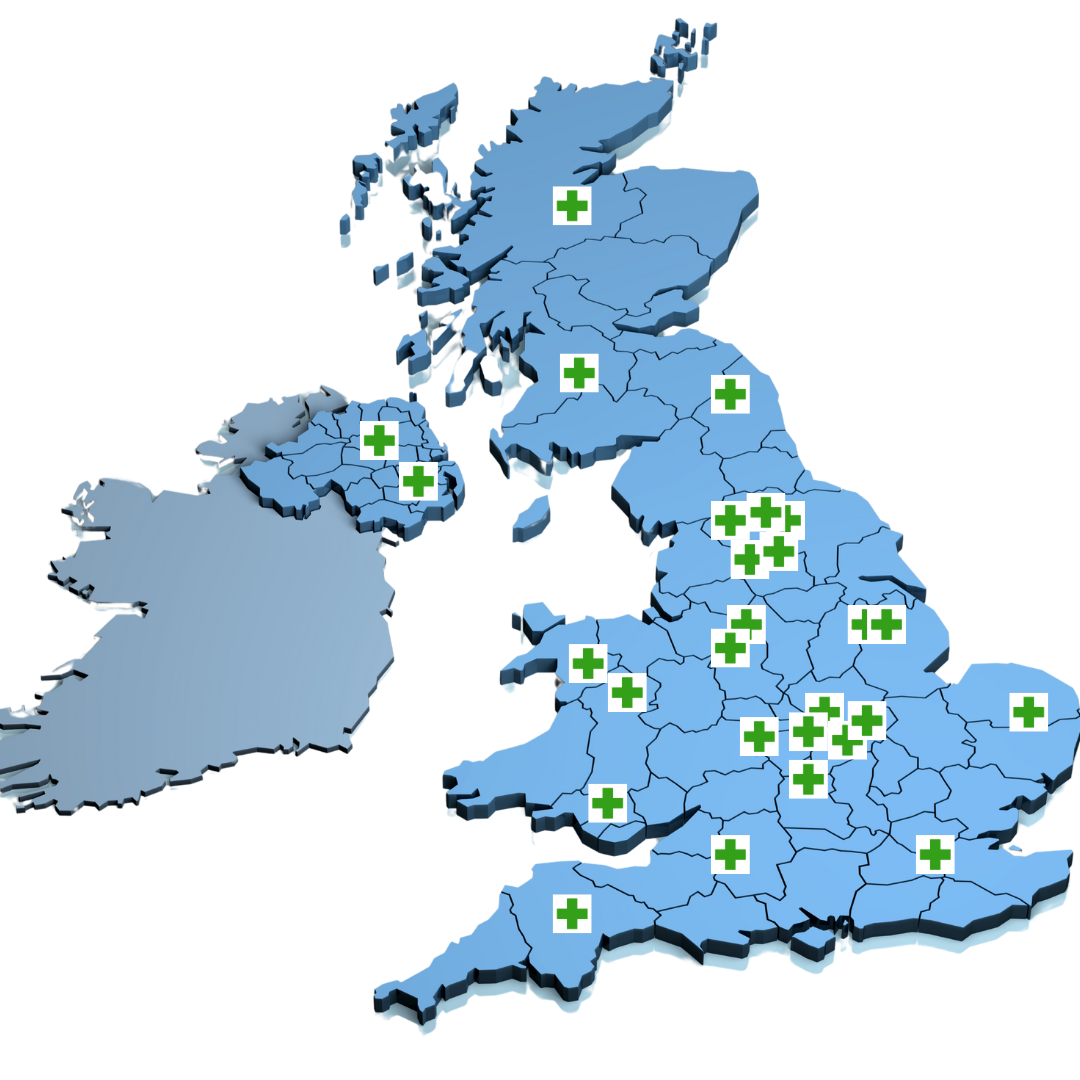
Having served the Ostomy community for over 25 years with support wear prescriptions, we have seen a lot of changes. More recently we are noticing more restrictions on what people can have prescribed but only in certain areas, and this is leading to growing gaps in allowances from region to region, which I'm sure you'll agree is unfair and unscientific not based on needs but on postcode. 
Of course, we all understand the NHS does not have limitless funds but what it does have needs to be managed properly. We believe strongly in the value of support wear not only through the better quality of life it gives the user (of course you might say we have a bias to say that since we provide that support wear) but for other reasons too.
An independent clinical trial conducted by Queens University Hospital London showed that using support wear in place of regular underwear did significantly improve quality of life scrore and very significantly reduced the incidence of hernias in the year of the trial. This fact alone should mean that by reducing hernias for the small cost of the support wear the NHS could prevent much more costly complications down the line. So this is one way that managing those funds properly with knowledge and insight into what it prescribes could be fixed. 
How might things change?
To try to answer this question let's first look at the current state of affairs when it comes to NHS provision of Stoma Support Wear. The main factors which influence prescribing decisions are:
- Clinical Need (Hernia Prevention & Management)
- The main justification for prescribing support garments is the risk of parastomal hernia, a common complication in ostomates.
- Those with a history of hernias or a high risk (e.g., due to previous abdominal surgery, obesity, or physical activity levels) are more likely to qualify.
- Individuals experiencing back pain or discomfort due to stoma-related posture changes may also be eligible.
- NHS Guidelines & Drug Tariff Restrictions
- Stoma support wear is included in Part IX of the NHS Drug Tariff, meaning it can be prescribed, but it is subject to restrictions.
- The amount and type of support wear allowed vary between NHS regions (Clinical Commissioning Groups, now part of Integrated Care Boards - ICBs).
- Some areas allow up to 6 pairs or more of support underwear per year, while others may only approve one support belt per year.
- Local Funding Decisions (Postcode Lottery)
- Some ICBs strictly limit prescriptions, while others are more flexible.
- Certain regions require an assessment by a stoma nurse before prescribing support wear, leading to inconsistencies.
- Some NHS Trusts refuse to prescribe at all, instead directing patients to buy garments privately.
- Stoma Nurse & GP Discretion
- While GP prescribing is technically possible, most GPs rely on stoma nurses to assess whether support wear is necessary.
- The interpretation of “need” can differ significantly between individual stoma nurses, leading to subjective decisions.

Key Issues & Inequalities:
- Postcode lottery: Patients in different areas receive vastly different levels of support.
- Lack of transparency: NHS guidance on support wear is not always clearly communicated.
- Financial burden: Those denied prescriptions must self-fund, which can be costly.
- Lack of standardization: There is no nationally enforced protocol for prescribing ostomy support wear.
How to Challenge a Decision:
- Request a stoma nurse assessment and ask them to justify any refusal based on clinical need.
- Check local ICB policies to understand your area's stance.
- Appeal to your GP, especially if you have a documented risk of hernia or discomfort.
- Seek advocacy support, such as from charities like Colostomy UK or the Ileostomy and Internal Pouch Association (IA).
So we can see where we are at right now and what may be happening in your area. So what does the future hold?
We believe education is key. Part of a stoma nurses training needs to include learning about accessories such as support wear that can aid an ostomy patient manage their stoma optimally. This would ensure an optimal quality of life with reduced complications. Such education would surely help nurses universally to be able to make more informed decisions around support wear needs.
More research is needed. More clinical trials to test the benefits of various levels of support wear would help clarify which type of support wear to prescribe when and how many garments are needed.
The recent abolition of NHS England 
As announced in the UK government's plans to integrate it into the Department of Health and Social Care (DHSC), could have an impact on prescribing rules, but the extent of the change will depend on how the transition is managed.
Potential Effects on Prescribing Rules for Ostomy Support Wear
- Greater Centralisation of Decision-Making
- NHS England currently oversees national policies, but Integrated Care Boards (ICBs) set prescribing rules at the local level.
- If NHS England is absorbed into DHSC, there is a chance for more standardised national guidelines, which could reduce regional discrepancies in ostomy support garment prescriptions.
- However, if power remains with ICBs, local variations (postcode lottery) in prescribing may persist.
- Changes in Funding Priorities
- The DHSC may review cost-saving measures as part of NHS restructuring.
- If prescribing policies are reassessed as part of a cost-cutting initiative, access to ostomy support wear could become stricter, requiring more justification for prescriptions.
- Alternatively, a more streamlined national framework might improve access by eliminating bureaucratic delays and ensuring more consistent eligibility criteria.
- ICBs and Local NHS Budgets
- Even if NHS England is abolished, ICBs will still control local healthcare budgets.
- If the government increases direct funding oversight, prescribing rules could become more uniform.
- However, if ICBs maintain significant autonomy, prescribing disparities across regions are unlikely to change significantly.
- Potential for a National Ostomy Care Framework
- The abolition of NHS England may push the government to reassess and unify policies for long-term condition management.
- A national framework for ostomy care could improve access to support wear, similar to efforts made in Scotland to create more standardised prescribing rules.
- If DHSC prioritises equity in care, it may lead to clearer guidance that removes the current postcode lottery.
What This Means for Ostomy Patients
- Short-Term: No immediate change, as policy shifts will take time to be implemented.
- Medium to Long-Term:
- If the government pushes for standardisation, patients may see more consistency in prescribing across different regions.
- If cost-cutting dominates, access to ostomy support wear may become more restricted.
So, in summary as you can see the NHS is a complicated beast, which despite it's incredible services does have it's faults. It always pains us to see some ostomy patients struggling with no support wear provision and no means to self fund. We are a small family business but will continue to try educating stoma nurses about support wear whenever we can.
We'd love to hear what you think about this topic.



I used to get ostomy products but a few years ago I was refused due to the fact I live in Scotland I now have to live with a herniated stoma which is very uncomfortable. I don’t know why they stopped me getting the proper underwear when I was getting it before?
Leave a comment